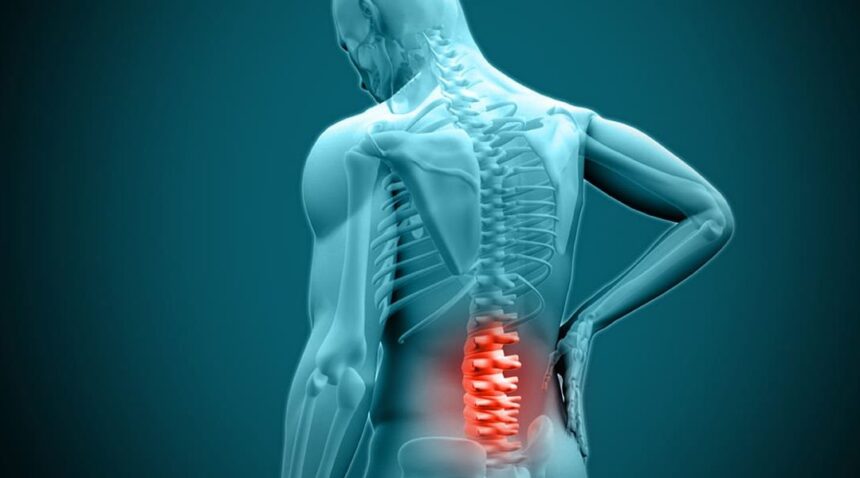
Disc surgery, also known as spinal disc surgery, is a medical procedure aimed at addressing issues related to intervertebral discs within the spinal column. These discs serve as cushions between the vertebrae, providing flexibility and absorbing shock. Complications such as herniation, degeneration, or impingement of nearby nerves can lead to significant pain, reduced mobility, and neurological symptoms. Disc surgery is typically an option when conservative treatments, including physical therapy and medication, fail to provide adequate relief. Here is more information on this surgery:
Understanding Disc Surgery
Disc surgery is typically explored when non-surgical methods do not address symptoms caused by certain conditions. These include herniated discs, degenerative disc disease, or spinal stenosis. Severe pain that persists beyond several weeks, loss of mobility, or neurological issues such as numbness or weakness may prompt further evaluation by a healthcare professional.
Spinal discs act as cushions between the vertebrae, absorbing shocks and maintaining spine flexibility. Damage or degeneration can lead to disc material pressing on nerves, resulting in pain or limited functionality. Surgery aims to correct these issues by relieving nerve pressure or stabilizing affected areas. Consulting a qualified spine specialist is necessary to determine if surgery aligns with your condition and symptoms.
Exploring Surgical Methods
The surgical approach depends on the condition and severity of symptoms. Common methods include:
- Discectomy removes the herniated portion of a disc to alleviate pressure on nearby nerves. This procedure helps reduce pain or restore sensation caused by nerve compression.
- Spinal Fusion involves connecting two or more vertebrae to stabilize sections of the spine affected by damaged discs. Bone grafts or implants are commonly used during this process.
- Laminectomy removes part of the vertebral bone or disc material to provide more space for spinal nerves. This method is often applied for cases involving spinal stenosis or persistent nerve compression.
Minimally invasive techniques may offer smaller incisions, shorter recovery periods, and reduced impact on surrounding tissues when compared to traditional open surgeries. A qualified surgeon evaluates these options based on imaging, symptoms, and overall health.
Identifying Benefits and Risks
Disc surgery may lead to significant pain relief, improved mobility, and enhanced quality of life. For some, regaining the ability to perform daily activities without debilitating pain becomes feasible after recovery. Early intervention in cases involving progressive nerve damage may also prevent long-term complications.
While this surgery can be highly effective, it is not without risks. Potential complications include infection, bleeding, or nerve damage. Success rates and recovery periods vary depending on the procedure and individual factors. Open communication with your surgeon provides clarity on realistic outcomes and potential risks.
Find a Neurosurgeon
Disc surgery plays a key role in treating severe spinal disc issues when conservative options prove insufficient. Procedures like discectomy, spinal fusion, or laminectomy target pressure on nerves and spinal stability to alleviate pain and restore functionality. These surgeries can greatly improve quality of life, but recovery time and potential complications should be investigated. While these techniques offer significant benefits, understanding risks and consulting with an experienced spine specialist enables an informed treatment decision.